9.3 Measuring and Improving Quality
Now that we have discussed the various ways that quality health care is defined, let’s discuss how quality care is measured, evaluated, and improved.
Utilization Review
Thinking back to value-based reimbursement models discussed in the “Health Care Economics” chapter, recall how quality performance measures relate to the reimbursement health care agencies receive from Medicare, Medicaid, and private insurance. A utilization review is an investigation of health care services performed by doctors, nurses, and other health care team members to ensure money is not wasted covering things that are unnecessary for proper treatment or are inefficient. Utilization review also allows organizations to objectively measure how their health care services and resources are being used to best meet their patients’ needs. Information from patients’ medical records are analyzed, along with patient demographics, to evaluate resource allocation, efficiency, and quality of health promotion initiatives.[1] See Figure 9.2[2] for an illustration of utilization review related to costs.

Using Informatics to Promote Quality
Utilization review relies on the collection of meaningful data from health records to analyze if quality metrics are being met. Informatics is defined by QSEN as using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.[3] Informatics allows members of the health care team to share, store, and analyze health-related information. Nurses have an important role in informatics. Nursing informatics is the science and practice of integrating nursing knowledge with information and communication technologies to promote the health of people, families, and communities worldwide.[4] See Figure 9.3[5] for an illustration of informatics.

These are several benefits of using informatics in health care:[6]
- Improvement of Patient Safety: Informatics allows for up-to-date information sharing by both the patient and members of the health care team. Using informatics can help to reduce the occurrence of medication errors, as well as monitor patient side effects and overall health status.
- Reduction of Delays in Care: Some health care informatics systems allow for direct communication between health care team members and the patients. The ability to ask and answer questions without needing to schedule an office appointment promotes the ability for care to be delivered in an efficient and reduced cost manner.
- Reduction of Waste: The use of informatics to share information between the care team members reduces waste associated with duplication of tests or exams when more than one provider is on the care team. Additionally, patients can request their records be shared with other health providers from other health organizations that helps to reduce duplication and unnecessary spending across the nation.
- Promotion of Patient Centered Care: Many informatics systems have “patient portal” options where the patient and/or designated personnel are able to be active participants in the care planning and health promotion processes. Informatics offers an inclusive environment for patients to communicate and share directly with their care team regardless of physical location and timing.
- Support of Quality Improvement: The continuous process of quality improvement requires the ability to collect and analyze data in a systematic and reliable manner. Using informatics provides members of the health care team a secure place to store data, as well as the ability to review in a timely manner.
Quality Indicators
Another way to measure quality is the National Database of Nursing Quality Indicators (NDNQI). NDNQI is a national nursing database that provides both quarterly and annual reports focused on evaluating quality in nursing care. Organizations who partner with NDNQI submit their data, often referred to as “nursing sensitive indicators,” that are compiled to form a national database. This database can be used to show a broad economic impact of the daily work being done by nurses.[7]
In collaboration with the American Nursing Association (ANA), the NDNQI established the database based on these original nurse-sensitive quality indicators:[8]
- Falls
- Falls with Injury
- Nursing Care Hours per Patient Day
- Skill Mix
- Pressure Ulcer Prevalence
- Hospital-Acquired Pressure Ulcer Prevalence
- RN Job Satisfaction
Since the development and utilization of the NDNQI quality indicators, nurses have been able to use this data in quality improvement practices and support their practice changes with evidence directly related to improved patient outcomes. The NDNQI database also allows health care teams to compare their organization’s data to other organizations across the nation. NDNQI also assists nursing researchers and nurse scientists by identifying gaps in the nursing practice and areas needing improvement.[9]
Quality Improvement
Quality Improvement (QI) is a systematic process using measurable data to improve health care services and the overall health status of patients.[10] QI is defined by QSEN as, “using data to monitor the outcomes of care processes and using improvement methods to design and test changes to continuously improve the quality and safety of health care systems.”[11]
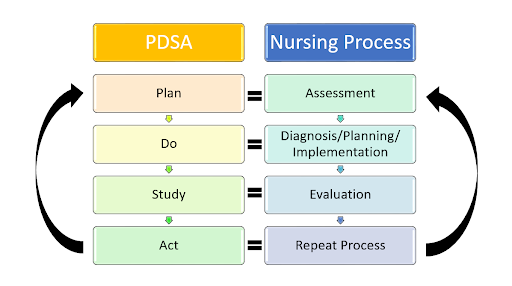
The overall goal of the QI process is to improve the quality and safety of health care. The process of quality improvement is very similar to the Nursing Process, but its purpose is to answer these three main questions:
- What are we trying to accomplish?
- How will we know if a change is an improvement?
- What changes can we make that will result in an improvement?
See Figure 9.4[12] for an illustration of the Quality Improvement Process.
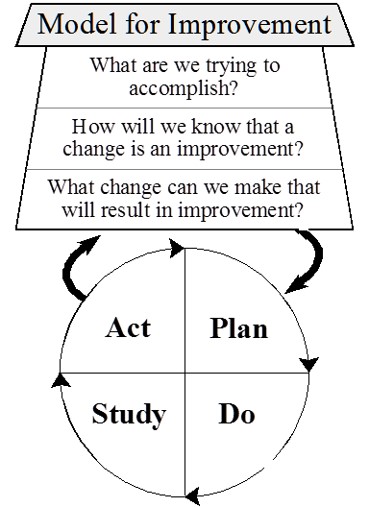
To answer these questions, QI is a continuous process that plans the project, implements interventions and collects data, studies the results, and evaluates the outcomes. The process is repeated after additional planning. During the QI process, four key steps are used to evaluate current patient care and evaluate if changes are needed. These components are referred to as Plan, Do, Study, and Act:
- Plan: The first step in the QI process is to identify what you will be testing or focusing on and what will be measured. Similar to the Nursing Process where subjective and objective data are collected, the nurse determines what qualitative and/or quantitative data will be needed during the QI process. The nurse also determines a time line for the QI project, such as one week for one year, including a specific framework for when data is collected and when it will be reviewed.
- Do: After the plan is determined, the nurse works with a health care team to implement the project and ensure data collection occurs.
- Study: During this phase, the nurse works with the health care team to review and analyze the data that was collected and determine if the outcomes were expected or not.
- Act: In the fourth step of the QI process, the team discusses the outcomes. In this step the team identifies barriers, strengths, weaknesses, and changes (if any) are needed in the nursing practice. The QI process is continuous, so the QI team uses the findings and continues the process of Plan, Do, and Study with the goals of ensuring high-quality and safe patient care.
See Figure 9.5[13] for an illustration comparing the QI process to the Nursing Process.
It is important to note that quality improvement is different from nursing research. QI evaluates processes in place and determines if changes are needed, whereas the goal of research is to identify new innovations in nursing practice.[14]
- Institute of Medicine (US) Committee on Utilization Management by Third Parties, Gray, B. H., & Field, M. J., (Eds.). (1989). Controlling costs and changing patient care? The role of utilization management. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK235000 ↵
- “Analyzing_Financial_Data_(5099605109).jpg” by Dave Dugdale is licensed under CC BY-SA 2.0 ↵
- Neumann, P. J., & Weinstein, M. C. (1991). The diffusion of new technology: Costs and benefits to health care. In Institute of Medicine (US) Committee on Technological Innovation in Medicine, Gelijns, A. C., & Halm, E. A. (Eds.). (1991). The changing economics of medical technology. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK234309/ ↵
- AMIA. (n.d.). Informatics: Research and practice. https://amia.org/about-amia/why-informatics/informatics-research-and-practice ↵
- “informatics-1322241_1920.jpg” by mariojsantos at Pixabay.com is licensed under CC0 ↵
- Otokiti, A. (2019). Using informatics to improve healthcare quality. Int J Health Care Qual Assur, 32(2), 425-430. https://doi.org/10.1108/ijhcqa-03-2018-0062 ↵
- Montalvo, I. (2007). The National Database of Nursing Quality Indicators (NDNQI). The Online Journal of Issues in Nursing, 12(3). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume122007/No3Sept07/NursingQualityIndicators.aspx ↵
- Montalvo, I. (2007). The National Database of Nursing Quality Indicators (NDNQI). The Online Journal of Issues in Nursing, 12(3). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume122007/No3Sept07/NursingQualityIndicators.aspx ↵
- Montalvo, I. (2007). The National Database of Nursing Quality Indicators (NDNQI). The Online Journal of Issues in Nursing, 12(3). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume122007/No3Sept07/NursingQualityIndicators.aspx ↵
- Study.com. (n.d.). What is economics? - Definition, history, timeline & importance [Video]. https://study.com/academy/lesson/what-is-economics-definition-history-timeline-importance.html ↵
- QSEN Institute. (n.d.). QSEN competencies: Quality improvement (QI). https://qsen.org/competencies/pre-licensure-ksas/#quality_improvement ↵
- “Model_for_Improvement.jpg” by Cliffnorman is licensed under CC BY-SA 4.0 ↵
- “Comparison_QI Process_Nursing Process.jpg” by Amy Tyznik, MPTC for Open RN is licensed under CC BY 4.0 ↵
- Agency for Healthcare Research and Quality. (2013, May). Module 4. Approaches to quality improvement. Practice facilitation handbook. https://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html ↵