10.7 QSEN: Advocating for Patient Safety and Quality Care in Nursing Education
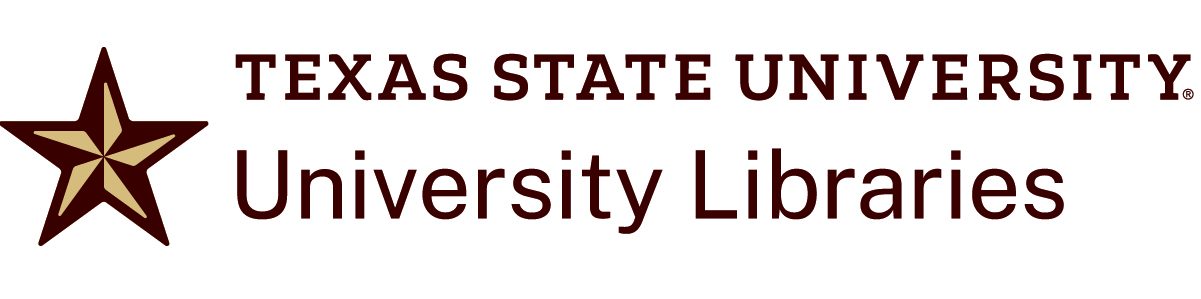
The Quality and Safety Education for Nurses (QSEN) project began advocating for safe, quality patient care in 2005 by defining six competencies for nursing graduates. This initiative was created after a decade of review and investigation into the high number and high cost of medical errors in the United States. The goal of the QSEN initiative was to prepare future nurses with the knowledge, skills, and attitudes (KSAs) needed to improve the quality and safety of the health care systems. Historically, nursing education focused on knowledge and skill acquisition, but did not address the attitudes and values of the nurse. The QSEN competencies are designed to train nursing students in KSAs as part of the pre-licensure nursing curriculum. The six QSEN competencies, as shown in Figure 10.6[1] are Patient-Centered Care, Teamwork and Collaboration, Evidence-Based Practice, Quality Improvement, Safety, and Informatics.[2]
Read the QSEN Pre-Licensure Table of Competencies.
View QSEN Institute’s Learning Modules Introduction YouTube video to learn more.[3]
Patient-Centered Care
The Patient-Centered Care QSEN competency advocates for the patient as “the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs.”[4] This competency encourages nurses to consider the clients’ cultural traditions and personal beliefs while providing compassionate care. Patient-centered care also includes the family in the care team. The goal of client-centered care is to improve individual client’s health outcomes. Integration of this competency has led to improved client satisfaction scores, reduced expenses, and a positive care environment.[5]
Teamwork and Collaboration
The Teamwork and Collaboration QSEN competency focuses on functioning effectively within nursing and interprofessional teams and fostering open communication, mutual respect, and shared decision-making to achieve quality patient care.[6] Effective communication has been proven to reduce errors and improve client safety.[7],[8] The Joint Commission also includes improved communication as one of the National Patient Safety Goals, aligning with this QSEN competency. Collaboration requires information sharing across disciplines with respect for the knowledge, skills, and experience of each team member. Two examples of tools used to promote effective teamwork and collaboration are ISBARR and TeamSTEPPS®. Additionally, “principles of collaboration” have been established by the ANA.
ISBARR
Several communication tools have been developed to improve communication in various health care settings such as ISBARR. ISBARR is a mnemonic for the components to include when communicating with another health care team member: Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.[9]
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the patient’s name and location, the reason you are calling, recent vital signs, and the status of the patient.
- Background: Provide pertinent background information about the patient such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current patient situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the patient, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the patient’s chart.
TeamSTEPPS®
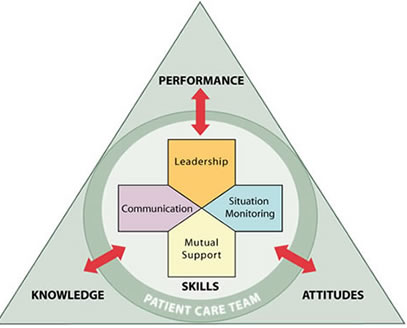
The Agency for Healthcare Research and Quality (AHRQ) developed the TeamSTEPPS®(Team Strategies and Tools to Enhance Performance and Patient Safety) tool kit to improve client safety through effective communication in health care environments. TeamSTEPPS® is an evidence-based framework consisting of four core competencies: communication, leadership, situation monitoring, and mutual support as illustrated in Figure 10.7.[10]
Read more about TeamSTEPPS®.
Read more about teamwork and collaboration in the “Collaboration Within the Interprofessional Team” chapter.
Principles of Collaboration
The American Nurses Association (ANA) and the American Organization of Nurse Executives (AONE) jointly created the “Principles of Collaboration” to guide nurses in creating, enhancing, and sustaining collaborative relationships. These principles include effective communication, authentic relationships, and a learning environment and culture. The principle of authentic relationships includes the following guidelines:[11]
- Be true to yourself – be sure your actions match your words and those around you are confident that what they see is what they get.
- Empower others to have ideas, to share those ideas, and to participate in projects that leverage or enact those ideas.
- Recognize and leverage each other’s strengths.
- Be honest 100% of the time – with yourself and with others.
- Respect others’ personalities, needs, and wants.
- Ask for what you want, but stay open to negotiating the difference.
- Assume good intent from others’ words and actions, and assume they are doing their best.
Read more about the “Principles of Collaboration” PDF by the ANA and AONE.
Evidence-Based Practice
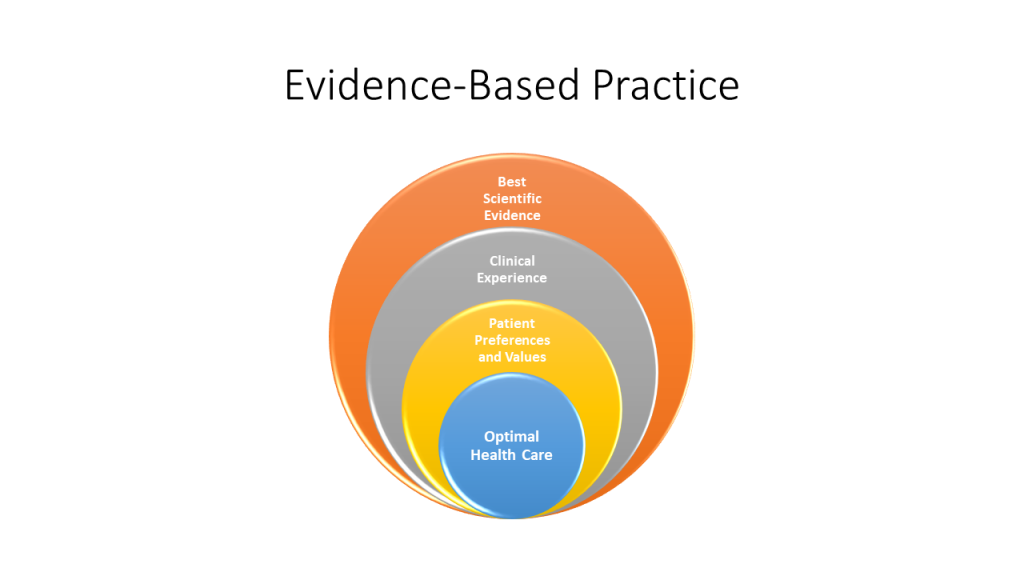
The Evidence-Based Practice QSEN competency focuses on integrating scientific evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care.[12] See Figure 10.8[13] for an illustration of Evidence-Based Practices (EBP). Read more about EPB in the “Quality” chapter. Read examples of evidence-based improvements in the following box.
Read these examples of evidence-based practice improvements:
Quality Improvement
The Quality Improvement QSEN competency focuses on using data to monitor the outcomes of care processes and using improvement methods to design and test changes to continuously improve the quality and safety of health care systems.[14] The goal of this competency is to improve processes, policies, and clinical decisions to improve client outcomes and system performance. As the pool of nursing literature grows and nursing practices have been updated to reflect current evidence, health care organizations have seen improvements in quality, safety, and experienced cost savings.[15]
Read more about the quality improvement processes in the “Quality and Evidence-Based Practice” chapter.
Safety
The Safety QSEN competency focuses on minimizing “risk of harm to patients and providers through both system effectiveness and individual performance.”[16] Although safety is embedded in all of the QSEN competencies, this competency specifically advocates for preventing client harm. Despite the health care industry’s continued focus on process improvement and improving client outcomes, errors continue to occur, and nurses are often involved in these events as frontline caregivers. Safe nursing practice starts with an awareness of the potential risks for client harm in every situation.
Several initiatives have been adopted to reduce risk for client harm, such as double-checking high-risk medications and verifying a patient’s name and date of birth prior to every intervention. However, client safety is compromised when there are gaps in quality measures such as inadequate staff training, broken equipment, or an organizational culture that doesn’t support best practices.
The “Safety” competency is best addressed by organizations establishing a safety culture where every worker commits to keeping client safety in the center of decision-making. An organization that has a culture of safety encourages reporting of unusual incidents, process failures, or other issues that could cause client harm, allowing the organization to investigate the event and take action to prevent the event from occurring in the future. Improvements are made as a result of a culture that questions attitudes, actions, and decisions in client care and recognizes threats to safety. Read more about safety culture in the “Legal Implications” chapter.
Informatics
The Informatics QSEN competency focuses on using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.[17] Health care is filled with various technologies used to promote a safe care environment, such as electronic medical records (EMRs), bedside medication administration devices, smart IV pumps, and medication distribution systems. These technologies provide safeguards and reminders to help prevent client harm, but the nurse must be knowledgeable in using technology, as well as understand how information obtained from technologies is used to improve client patient outcomes. As information related to technology continues to evolve, it is the responsibility of every nurse to participate in continued professional development related to informatics.
- “QSEN Competencies.png" by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- QSEN. (n.d.). About.https://qsen.org/about-qsen/ ↵
- QSEN Institute. (2012, November 5). QSEN learning modules introduction. [Video]. YouTube. All rights reserved. https://youtu.be/Y3MrYFRQRo8 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- Roseman, D., Osborne-Stafsnes, J., Amy, C. H., Boslaugh, S., & Slate-Miller, K. (2013). Early lessons from four 'aligning forces for quality' communities bolster the case for patient-centered care. Health Aff (Millwood), 32(2), 232-241. https://doi.org/10.1377/hlthaff.2012.1085 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- Burgener, A. M. (2020). Enhancing communication to improve patient safety and to increase patient satisfaction. The Health Care Manager, 39(3), 128-132. https://doi.org/10.1097/hcm.0000000000000298 ↵
- Shitu, Z., Hassan, I., Aung, M. M. T., Tuan Kamaruzaman, T. H., & Musa, R. M. (2018). Avoiding medication errors through effective communication in a healthcare environment. Malaysian Journal of Movement, Health & Exercise, 7(1), 115-128. https://doi.org/10.15282/mohe.v7i1.202 ↵
- Enlow, M., Shanks, L., Guhde, J., & Perkins, M. (2010). Incorporating interprofessional communication skills (ISBARR) into an undergraduate nursing curriculum. Nurse Educator, 35(4), 176-180. https://doi.org/10.1097/nne.0b013e3181e339ac ↵
- AHRQ. (n.d.). TeamSTEPPS. https://www.ahrq.gov/teamstepps/index.html ↵
- American Nurses Association & American Organization of Nurses Executives. (n.d.). ANA/AONE principles for collaborative relationships between clinical nurses and nurse managers. https://www.nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principles-of-collaborative-relationships.pdf ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- "Evidence-Based Practice.jpg" by Kim Ernstmeyer for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- Cullen, L., Titler, M. G., & Rempel, G. (2011). An advanced educational program promoting evidence-based practice. Western Journal of Nursing Research, 33(3), 345-364. https://doi.org/10.1177/0193945910379218 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵