3.2 Communication
Effective communication is a vital component of effective assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA).[1]
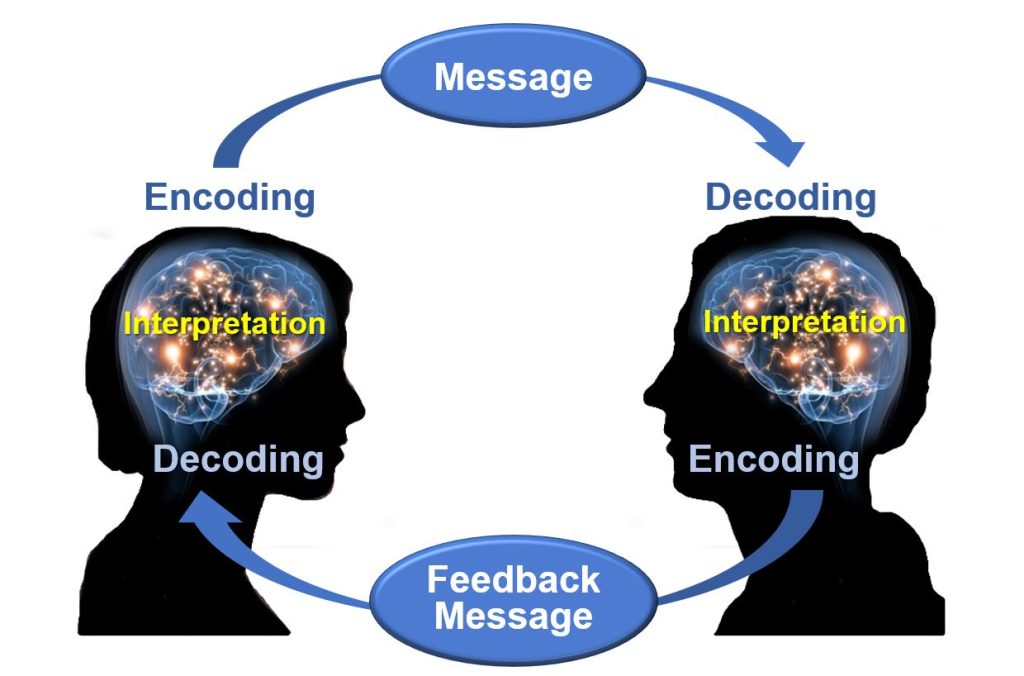
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1 for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
Closed-loop communication is vital for communication among health care team members to avoid misunderstanding that can cause unsafe client care. According to the HIPAA Journal, poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.”[2] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. Expressing clarity when providing direction is integral. A lack of clarity will lead to misunderstanding, unfinished tasks, incomplete care, and medical errors.[3]
Effective communication is at the heart of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs often change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift:
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task but excessive or irrelevant information should be avoided. Excessive or irrelevant information can confuse the listener and waste precious time.
- Correct: Correct communication is not cloudy or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act.
- Complete: Complete instructions leave no room for doubt. Assuming a nursing team member knows what to do and how to do it, along with what information to report and when, can create havoc and frustration for both staff and clients.[4]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider during a medical emergency. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN carrying out the order confirms hearing, understanding, and completing the order by repeating back, “Epinephrine 1 mg/mL IV push was given now.” Health care team members participating in this verbal exchange of information ensure unit functioning while also focusing on achieving desired client outcomes.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- HIPAA Journal. (n.d.). Effects of poor communication in healthcare. https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/ ↵
- HIPAA Journal. (n.d.). Effects of poor communication in healthcare. https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/ ↵
- LaCharity, L. A., Kumagai, C. K., & Bartz, B. (2019). Prioritization, delegation and assignment (4th ed.). Mosby, p. 6. ↵
A process that enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly.