7.6 Teams and Teamwork
Now that we have reviewed the first three IPEC competencies related to valuing team members, understanding team members’ roles and responsibilities, and using structured interprofessional communication strategies, let’s discuss strategies that promote effective teamwork. The fourth IPEC competency states, “Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable.”[1] See the following box for the components of this IPEC competency.
Components of IPEC’s Teams and Teamwork Competency[2]
- Describe the process of team development and the roles and practices of effective teams.
- Develop consensus on the ethical principles to guide all aspects of teamwork.
- Engage health and other professionals in shared patient-centered and population-focused problem-solving.
- Integrate the knowledge and experience of health and other professions to inform health and care decisions, while respecting patient and community values and priorities/preferences for care.
- Apply leadership practices that support collaborative practice and team effectiveness.
- Engage self and others to constructively manage disagreements about values, roles, goals, and actions that arise among health and other professionals and with patients, families, and community members.
- Share accountability with other professions, patients, and communities for outcomes relevant to prevention and health care.
- Reflect on individual and team performance for individual, as well as team, performance improvement.
- Use process improvement to increase effectiveness of interprofessional teamwork and team-based services, programs, and policies.
- Use available evidence to inform effective teamwork and team-based practices.
- Perform effectively on teams and in different team roles in a variety of settings.
Developing effective teams is critical for providing health care that is patient-centered, safe, timely, effective, efficient, and equitable.[3] See Figure 7.5[4] for an image illustrating interprofessional teamwork.

Nurses collaborate with the interprofessional team by not only assigning and coordinating tasks, but also by promoting solid teamwork in a positive environment. A nursing leader, such as a charge nurse, identifies gaps in workflow, recognizes when task overload is occurring, and promotes the adaptability of the team to respond to evolving patient conditions. Qualities of a successful team are described in the following box.[5]
Qualities of A Successful Team[6]
- Promote a respectful atmosphere
- Define clear roles and responsibilities for team members
- Regularly and routinely share information
- Encourage open communication
- Implement a safety culture
- Provide clear directions
- Share responsibility for team success
- Balance team member participation for the situations occurring
- Acknowledge and manage conflict
- Enforce accountability
- Communicate the decision-making process
- Facilitate access to needed resources
- Evaluate team outcomes and adjust as needed
TeamSTEPPS®
TeamSTEPPS® is an evidence-based framework used to optimize team performance across the health care system. It is a mnemonic standing for Team Strategies and Tools to Enhance Performance and Patient Safety. The Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense (DoD) developed the TeamSTEPPS® framework as a national initiative to improve patient safety by improving teamwork skills and communication.[7]
View this video about the TeamSTEPPS® framework[8]:
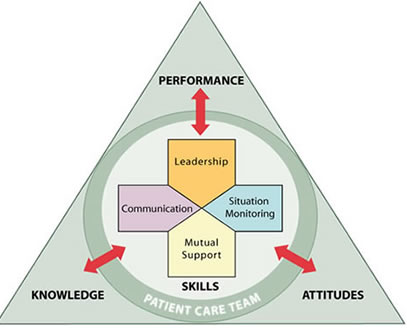
TeamSTEPPS® is based on establishing team structure and four teamwork skills: communication, leadership, situation monitoring, and mutual support.[9] See Figure 7.6[10] for an image of the TeamSTEPPS® framework followed by a description of each TeamSTEPPS® skill. The components of this model are described in the following sections.
Team Structure
A nursing leader establishes team structure by assigning or identifying team members’ roles and responsibilities, holding team members accountable, and including clients and families as part of the team.
Communication
Communication is the first skill of the TeamSTEPPS® framework. As previously discussed, it is defined as a “structured process by which information is clearly and accurately exchanged among team members.” All team members should use these skills to ensure accurate interprofessional communication:
- Provide brief, clear, specific, and timely information to other team members.
- Seek information from all available sources.
- Use ISBARR and handoff techniques to communicate effectively with team members.
- Use closed-loop communication to verify information is communicated and completed.
- Document appropriately to facilitate continuity of care across interprofessional team members.
These communication strategies are further described in the “Interprofessional Communication” section of this chapter.
Leadership
Leadership is the second skill of the TeamSTEPPS® framework. As previously discussed, it is defined as the “ability to maximize the activities of team members by ensuring that team actions are understood, changes in information are shared, and team members have the necessary resources.” An example of a nursing team leader in an inpatient setting is the charge nurse.
Effective team leaders demonstrate the following responsibilities:[11]
- Organize the team.
- Identify and articulate clear goals (i.e., share the plan).
- Assign tasks and responsibilities.
- Monitor and modify the plan and communicate changes.
- Review the team’s performance and provide feedback when needed.
- Manage and allocate resources.
- Facilitate information sharing.
- Encourage team members to assist one another.
- Facilitate conflict resolution in a learning environment.
- Model effective teamwork.
Three major leadership tasks include sharing a plan, monitoring and modifying the plan according to situations that occur, and reviewing team performance. Tools to perform these tasks are discussed in the following subsections.
Sharing the Plan
Nursing team leaders identify and articulate clear goals to the team at the start of the shift during inpatient care using a “brief.” The brief is a short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies. See a Brief Checklist in the following box.[12]
Brief Checklist
During the brief, the team should address the following questions:[13]
___ Who is on the team?
___ Do all members understand and agree upon goals?
___ Are roles and responsibilities understood?
___ What is our plan of care?
___ What are staff and provider’s availability throughout the shift?
___ How is workload shared among team members?
___ What resources are available?
Monitoring and Modifying the Plan
Throughout the shift, it is often necessary for the nurse leader to modify the initial plan as patient situations change on the unit. A huddle is a brief meeting during a shift to reestablish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed. Read more about situational awareness in the “Situation Monitoring” subsection below..
Reviewing the Team’s Performance
When a significant or emergent event occurs during a shift, such as a “code,” it is important to later review the team’s performance and reflect on lessons learned by holding a “debrief” session. A debrief is an informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflecting on lessons learned.[14] See the following box for a Debrief Checklist.
Debrief Checklist[15]
The team should address the following questions during a debrief:
___ Was communication clear?
___ Were roles and responsibilities understood?
___ Was situation awareness maintained?
___ Was workload distribution equitable?
___ Was task assistance requested or offered?
___ Were errors made or avoided?
___ Were resources available?
___ What went well?
___ What should be improved?
Situation Monitoring
Situation monitoring is the third skill of the TeamSTEPPS® framework and defined as the “process of actively scanning and assessing situational elements to gain information or understanding, or to maintain awareness to support team functioning.” Situation monitoring refers to the process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you. Situation awareness refers to a team member knowing what is going on around them. The team leader creates a shared mental model to ensure all team members have situation awareness and are “on the same page” as situations evolve on the unit. The STEP tool is used by team leaders to assist with situation monitoring.[16]
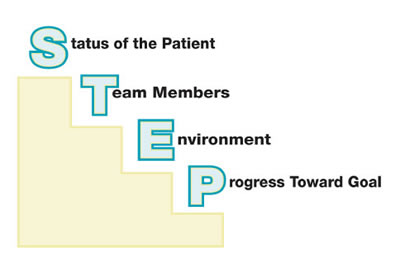
STEP
The STEP tool is a situation monitoring tool used to know what is going on with you, your patients, your team, and your environment. STEP stands for Status of the patients, Team members, Environment, and Progress Toward Goal. See an illustration of STEP in Figure 7.7.[17] The components of the STEP Tool are described in the following box.[18]
STEP Tool[19]
Status of Patients: “What is going on with your patients?”
__ Patient History
__ Vital Signs
__ Medications
__ Physical Exam
__ Plan of Care
__ Psychosocial Issues
Team Members: “What is going on with you and your team?”(See the “I’M SAFE Checklist” below.)
__ Fatigue
__ Workload
__ Task Performance
__ Skill
__ Stress
Environment: Knowing Your Resources
__ Facility Information
__ Administrative Information
__ Human Resources
__ Triage Acuity
__ Equipment
Progression Towards Goal: (See “Briefs,” “Huddles,” and “Debriefs” in the “Leadership” section.)
__ Status of the Team’s Patients
__ Established Goals of the Team
__ Tasks/Actions of the Team
__ Appropriateness of the Plan – Are Modifications Needed?
Cross Monitoring
As the STEP tool is implemented, the team leader continues to cross monitor to reduce the incidence of errors. Cross monitoring includes the following:[20]
- Monitoring the actions of other team members.
- Providing a safety net within the team.
- Ensuring that mistakes or oversights are caught quickly and easily.
- “Watching each other’s back.”
I’M SAFE Checklist
The I’M SAFE mnemonic is a tool used to assess one’s own safety status, as well as that of your team members in their ability to provide safe patient care. See the I’M SAFE Checklist in the following box.[21] If a team member feels their ability to provide safe care is diminished because of one of these factors, they should notify the charge nurse or other nursing supervisor. In a similar manner, if a nurse notices that another member of the team is impaired or providing care in an unsafe manner, it is an ethical imperative to protect clients and report their concerns according to agency policy.[22]
I’m SAFE Checklist[23]
__ I: Illness
__M: Medication
__S: Stress
__A: Alcohol and Drugs
__F: Fatigue
__E: Eating and Elimination
Read an example of a nursing team leader performing situation monitoring using the STEP tool in the following box.
Example of Situation Monitoring
Two emergent situations occur simultaneously on a busy medical-surgical hospital unit as one patient codes and another develops a postoperative hemorrhage. The charge nurse is performing situation monitoring by continually scanning and assessing the status of all patients on the unit and directing additional assistance where it is needed. Each nursing team member maintains situation awareness by being aware of what is happening on the unit, in addition to caring for the patients they have been assigned. The charge nurse creates a shared mental model by ensuring all team members are aware of their evolving responsibilities as the situation changes. The charge nurse directs additional assistance to the emergent patients while also ensuring appropriate coverage for the other patients on the unit to ensure all patients receive safe and effective care.
For example, as the “code” is called, the charge nurse directs two additional nurses and two additional assistive personnel to assist with the emergent patients while the other nurses and assistive personnel are directed to “cover” the remaining patients, answer call lights, and assist patients to the bathroom to prevent falls. Additionally, the charge nurse is aware that after performing a few rounds of CPR for the coding patient, the assistive personnel must be switched with another team member to maintain effective chest compressions. As the situation progresses, the charge nurse evaluates the status of all patients and makes adjustments to the plan as needed.
Mutual Support
Mutual support is the fourth skill of the TeamSTEPPS® framework and defined as the “ability to anticipate and support team members’ needs through accurate knowledge about their responsibilities and workload.” Mutual support includes providing task assistance, giving feedback, and advocating for patient safety by using assertive statements to correct a safety concern. Managing conflict is also a component of supporting team members’ needs.
Task Assistance
Helping other team members with tasks builds a strong team. Task assistance includes the following components:[24]
- Team members protect each other from work-overload situations.
- Effective teams place all offers and requests for assistance in the context of patient safety.
- Team members foster a climate where it is expected that assistance will be actively sought and offered.
Example of Task Assistance
In a previous example, one patient on the unit was coding while another was experiencing a postoperative hemorrhage. After the emergent care was provided and the hemorrhaging patient was stabilized, Sue, the nurse caring for the hemorrhaging patient, finds many scheduled medications for her other patients are past due. Sue reaches out to Sam, another nurse on the team, and requests assistance. Sam agrees to administer a scheduled IV antibiotic to a stable third patient so Sue can administer oral medications to her remaining patients. Sam knows that on an upcoming shift, he may need to request assistance from Sue when unexpected situations occur. In this manner, team members foster a climate where assistance is actively sought and offered to maintain patient safety.
Feedback
Feedback is provided to a team member for the purpose of improving team performance. Effective feedback should follow these parameters:[25]
- Timely: Provided soon after the target behavior has occurred.
- Respectful: Focused on behaviors, not personal attributes.
- Specific: Related to a specific task or behavior that requires correction or improvement.
- Directed towards improvement: Suggestions are made for future improvement.
- Considerate: Team members’ feelings should be considered and privacy provided. Negative information should be delivered with fairness and respect.
Advocating for Safety with Assertive Statements
When a team member perceives a potential patient safety concern, they should assertively communicate with the decision maker to protect patient safety. This strategy holds true for ALL team members, no matter their position within the hierarchy of the health care environment. The message should be communicated to the decision maker in a firm and respectful manner using the following steps:[26]
- Make an opening.
- State the concern.
- State the problem (real or perceived).
- Offer a solution.
- Reach agreement on next steps.
Examples of Using Assertive Statements to Promote Patient Safety
A nurse notices that a team member did not properly wash their hands during patient care. Feedback is provided immediately in a private area after the team member left the patient room: “I noticed you didn’t wash your hands when you entered the patient’s room. Can you help me understand why that didn’t occur?” (Wait for an answer.) “Performing hand hygiene is essential for protecting our patients from infection. Here is a handout from the CDC that explains when hand hygiene should occur and how to properly perform hand hygiene. Let me know if you have any questions and I will check back with you later in the shift.” (Monitor the team member for appropriate hand hygiene for the remainder of the shift.)
Two-Challenge Rule
When an assertive statement is ignored by the decision maker, the team member should assertively voice their concern at least two times to ensure that it has been heard by the decision maker. This strategy is referred to as the two-challenge rule. When this rule is adopted as a policy by a health care organization, it empowers all team members to pause care if they sense or discover an essential safety breach. The decision maker being challenged is expected to acknowledge the concern has been heard.[27]
CUS Assertive Statements
During emergent situations, when stress levels are high or when situations are charged with emotion, the decision maker may not “hear” the message being communicated, even when the two-challenge rule is implemented. It is helpful for agencies to establish assertive statements that are well-recognized by all staff as implementation of the two-challenge rule. These assertive statements are referred to as the CUS mnemonic: “I am Concerned – I am Uncomfortable – This is a Safety issue!”[28] See Figure 7.8[29] for an illustration of CUS Assertive Statements.

Using these scripted messages may effectively catch the attention of the decision maker. However, if the safety issue still isn’t addressed after the second statement or the use of “CUS” assertive statements, the team member should take a stronger course of action and utilize the agency’s chain of command. For the two-challenge rule and CUS assertive statements to be effective within an agency, administrators must support a safety culture and emphasize the importance of these initiatives to promote patient safety.
Read an example of a nurse using assertive statements in the following box.
Assertive Statement Example
A nurse observes a new physician resident preparing to insert a central line at a patient’s bedside. The nurse notes the resident has inadvertently contaminated the right sterile glove prior to insertion.
Nurse: “Dr. Smith, I noticed that you contaminated your sterile gloves when preparing the sterile field for central line insertion. I will get a new set of sterile gloves for you.”
Dr. Smith: (Ignores nurse and continues procedure.)
Nurse: “Dr. Smith, please pause the procedure. I noticed that you contaminated your right sterile glove by touching outside the sterile field. I will get a new set of sterile gloves for you.”
Dr. Smith: “My gloves are fine.” (Prepares to initiate insertion.)
Nurse: “Dr. Smith – I am concerned! I am uncomfortable! This is a safety issue!”
Dr. Smith: (Stops procedure, looks up, and listens to the nurse.) “I’ll wait for that second pair of gloves.”
Managing Conflict
Conflict is not uncommon on interprofessional teams, especially when there are diverse perspectives from multiple staff regarding patient care. Nurse leaders must be prepared to manage conflict to support the needs of their team members.
When conflict occurs, the DESC Tool can be used to help resolve conflict by using “I statements.” DESC is a mnemonic that stands for the following:[30]
- D: Describe the specific situation or behavior; provide concrete data.
- E: Express how the situation makes you feel/what your concerns are using “I” messages.
- S: Suggest other alternatives and seek agreement.
- C: Consequences stated in terms of impact on established team goals while striving for consensus.
The DESC tool should be implemented in a private area with a focus on WHAT is right, not WHO is right. Read an example of a nurse using the DESC Tool in the following box.
Example of Using the DESC Tool[31]
Situation: A physician became angry at a nurse who was inserting a patient’s Foley catheter and yelled at the nurse in front of the patient and other team members. The nurse later addressed the physician in a private area outside the patient’s room using the DESC Tool and “I statements”:
D: “I noticed you got angry at me when I inserted the patient’s Foley catheter.”
E: “I’m concerned how you addressed that concern in front of the patient and three other staff members. It made me feel bad in front of the patient and my colleagues.”
S: “In the future, if you have an issue with how I do things, please pull me aside privately to discuss your concern.”
C: “If we can’t agree on this alternative, we’ll have to take this to the next level.”
Managing interpersonal conflict resolution is described further in the “Conflict Resolution” section.
View a detailed video webinar describing the TeamSTEPPS® principles.[32]
- Interprofessional Education Collaborative. IPEC core competencies. https://www.ipecollaborative.org/ipec-core-competencies ↵
- Interprofessional Education Collaborative. IPEC core competencies. https://www.ipecollaborative.org/ipec-core-competencies ↵
- Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report on an expert panel. Interprofessional Education Collaborative. https://ipec.memberclicks.net/assets/2011-Original.pdf ↵
- "400845937-huge.jpg" by Flamingo Images is used under license from Shutterstock.com ↵
- O’Daniel, M., & Rosenstein, A. H. (2011). Professional communication and team collaboration. In: Hughes R.G. (Ed.). Patient safety and quality: An evidence-based handbook for nurses. Agency for Healthcare Research and Quality (US); Chapter 33. https://www.ncbi.nlm.nih.gov/books/NBK2637 ↵
- O’Daniel, M., & Rosenstein, A. H. (2011). Professional communication and team collaboration. In: Hughes R.G. (Ed.). Patient safety and quality: An evidence-based handbook for nurses. Agency for Healthcare Research and Quality (US); Chapter 33. https://www.ncbi.nlm.nih.gov/books/NBK2637 ↵
- AHRQ. (2019, June). TeamSTEPPS 2.0. https://www.ahrq.gov/teamstepps/instructor/index.html ↵
- AHRQ Patient Safety. (2015, April 29). TeamSTEPPS overview. [Video]. YouTube. All rights reserved. https://youtu.be/p4n9xPRtSuU ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- “tslogo1med.jpg” by unknown author is in the Public Domain. Access for free at https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html. ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- “stepfig1.jpg” by unknown author is in the Public Domain. Access for free at https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html. ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- “cusfig1.jpg” by unknown author is in the Public Domain. Access for free at https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html. ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ Patient Safety. (2017, July 26). Introduction to the fundamentals of TeamSTEPPS® concepts and tools. [Video]. YouTube. Video in the Public Domain. https://youtu.be/fxlRtpzsUug ↵
A short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies.
A brief meeting during a shift to reestablish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed.
An informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflecting on lessons learned after a significant event occurs.
The process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you.
The awareness of a team member knowing what is going on around them.
The actions of a team leader that ensure all team members have situation awareness and are "on the same page" as situations evolve on the unit.